With over three decades of NHS experience, Simon Hepworth, Head of Customer Success at EBO, brings a deep understanding of the challenges and opportunities within UK healthcare. Having led national programmes such as the Digital Waiting List Validation and Patient Engagement Portals for NHS England, Simon has witnessed first-hand the evolving complexity of patient engagement, capacity management, and digital transformation across the health system.
At EBO, Simon channels that experience into helping NHS Trusts and ICBs implement AI-powered Waiting List Validation and Optimisation solution ,empowering healthcare teams to engage patients proactively, improve data accuracy, and reduce administrative burden.
Below, Simon shares his perspective on how digital innovation and automation are redefining the way the NHS manages waiting lists, ensuring efficiency, safety, and equity for all patients.
1. What are the biggest challenges the NHS currently faces in managing and validating waiting lists?
The NHS is tackling a scale and complexity issue that traditional methods simply can’t keep pace with. Lists are dynamic, changing daily, and spread across fragmented systems. Workforce shortages mean we can’t rely on manual validation, and patient contact data is often outdated or incomplete.
There’s also an equity challenge: not every patient can easily be reached or engaged through standard channels. The biggest opportunity lies in building smarter, automated, and inclusive systems that can manage this complexity safely, consistently, and at scale.
2. What lessons did you learn from the early national pilots of digital waiting list validation?
Early pilots proved that technology alone isn’t the answer, success depends on design simplicity and patient trust. The most effective programmes used clear messaging, multiple communication channels, and real-time data integration to avoid duplication and errors. We also learned that patients respond better to personalised communication. Digital solutions without automation and integration capabilities place additional pressures on the workforce.
3. How has the NHS’ approach to waiting list validation evolved over the past few years?
We’ve shifted from viewing validation as a one-off administrative clean-up to treating it as a continuous operational discipline. It’s now embedded in elective recovery planning, with digital engagement on 12-week cycles.
4. How has the NHS England Elective Recovery Plan influenced the way Trusts now think about validation, engagement, and capacity optimisation?
The Elective Recovery Plan made validation a strategic enabler of recovery, linking it directly to access, utilisation, and patient experience. It pushed organisations to think beyond backlog reduction, towards smarter demand management, capacity optimisation, and proactive patient engagement. Validation is no longer about tidying data; it’s about improving system flow, equity, and clinical prioritisation.
5. Why do you believe AI and automation can play a meaningful role in addressing this challenge?
Because they can handle the volume, variability, and nuance of NHS waiting lists in ways that manual processes can’t.
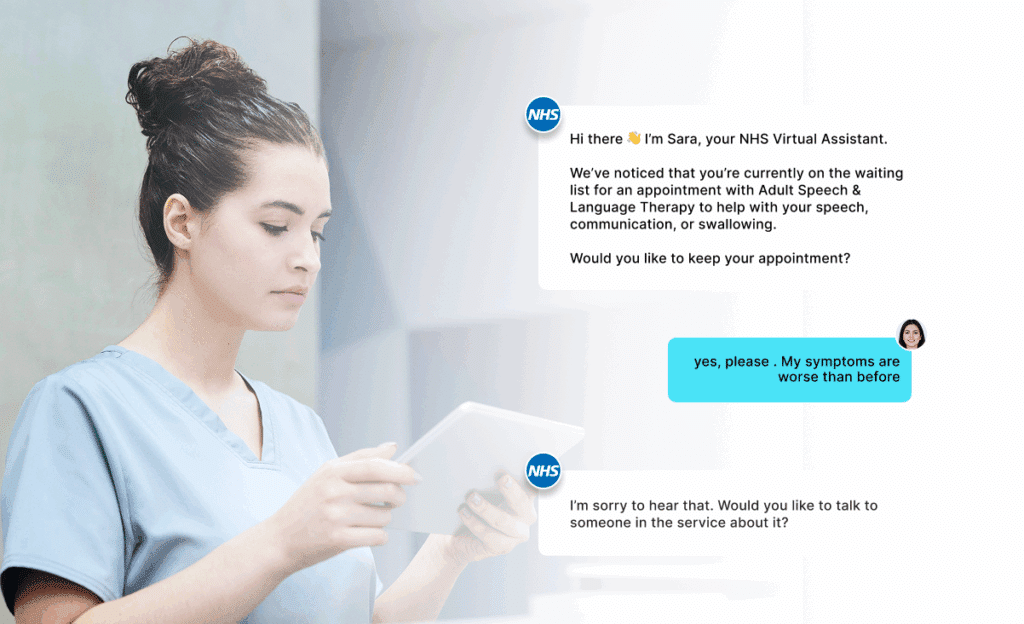
AI enables two-way patient engagement at scale, understanding free-text responses, adapting tone and language, and routing complex cases to humans. Automation ensures data consistency, auditability, and efficiency, freeing staff to focus on care rather than repetitive admin.
6. What kind of measurable improvements have been seen from digital or AI-led validation so far?
Across the system, Trusts are reporting significant time savings, higher response and confirmation rates, and more accurate data feeding into operational planning.
We’re seeing validation cycles that once took months completed in days, and meaningful reductions in long-wait backlogs as patients who no longer need care are identified quickly. Just as importantly, patients are reporting better experiences, they feel informed, involved, and able to update their preferences easily.
7. How do clinicians and staff perceive this new model — supportive or disruptive?
Most describe it as supportive once it’s embedded. Initially there’s understandable caution, any digital change can feel like a risk to established workflows, but when staff see that it removes repetitive tasks and provides cleaner, more actionable data, it quickly gains support.
Clinical teams value the safety and transparency of digital validation when designed with proper escalation, audit trails, and governance. It’s increasingly seen as an enabler, not a replacement.
8. In your view, what does the future of waiting list validation look like in the next 3–5 years?
We’ll see validation become continuous, intelligent, and patient-led. Data will refresh automatically through ongoing engagement cycles; AI will detect patterns, predict risks, and prompt timely interventions; and integration with EPRs will make validation a live part of care coordination.
We’ll also see stronger equity monitoring, ensuring every patient, regardless of language, digital literacy, or background, has an equal opportunity to engage and be heard.
9. What advice would you give to NHS leaders considering digital or AI-based validation for the first time?
- Start small but design for scale. Define your cohorts and outcomes clearly. Build governance early, safety, IG, and escalation need to be integral.
- Co-design with patients, clinicians and operational teams to build trust and accessibility. Integrate, don’t duplicate validation must connect to core systems, not sit beside them.
- And finally, measure what matters: equity, response quality, and conversion to care, not just numbers contacted.
10. What excites you most about the potential of AI to improve patient engagement and operational efficiency in the NHS?
It’s the ability to make healthcare more human, not less.
AI allows the NHS to communicate personally with every patient, understand their needs in real time, and act quickly, all without overburdening staff. It’s about creating smarter systems that learn, stronger insights that guide, and better care that’s equitable and efficient.
That’s what digital transformation in the NHS should ultimately deliver.
Simon Hepworth’s insight reflects a critical shift in the NHS, from reactive backlog management to proactive, intelligent patient engagement. As Trusts and ICBs continue to face increasing operational and workforce pressures, AI-powered waiting list validation offers a path forward: one that delivers efficiency, consistency, and fairness at scale.